Clinical Trials: ICH, GCP rules, regulatory (EMEA, FDA) GCP inspections. Key documents.
GCP training on-line (GCP certification)
1) GCP course for Investigators and CRAs
2) GCP course for Auditors
(see below or for detailed information click here)
GCP training curriculum
(1) GCP training for Beginners
ICH-GCP (E6-R2) international guideline
1: Introduction to GCP
1.1 Background
1.2 What is GCP
1.3 New GCP Guide
1.4 The Principles of ICH GCP
1.5 Some General Point
1.6 Documentation and Version Control
1.7 Quality Assurance
2: Competent Authorities (CA) and Independent Ethics Committee
2.1 Responsibilities of the CRA
2.2 Responsibility of the IEC
2.3 Subject Informed Consent Forms
2.4 Composition, Functions, Operations, Procedures and Records
3: Investigators
3.1 Investigator Responsibilities
3.2 Investigator Qualifications and Agreements
3.3 Adequate Resource
3.4 Medical Care of Trial Subjects
3.5 Communication with IRB/IEC
3.6 Compliance with the Protocol
3.7 Investigational Medicinal Products
3.8 Randomization Procedures and Un-blinding
3.9 Informed Consent of Trial Subject
3.10 Records and Reports
3.11 Premature Termination or Suspension of a Trial
3.12 Progress Reports and Final Report(s) by Investigator
3.13 Archiving
3.14 Considerations for the use of electronic systems in clinical trial management
3.15 Updated information on electronic records and use of EMRs in clinical research.
4: Sponsor’s Responsibilities
4.1 Quality Assurance and Quality Control
4.2 Contract Research Organization
4.3 Trial Design
4.4 Trial Management, Data Handling and Record Keeping
4.5 Investigator Selection
4.6 Financing
4.7 Notification/ Submission to Regulatory Authorities
4.8 Gaining CA approval in the EU
4.9 Confirmation of Review by IRB/IEC
4.10 Information on IM
4.11 Manufacturing, Packaging, Labelling and Coding Investigational Products
4.12 Supplying and Handling Investigational Products
4.13 Record Access
4.14 Audit and Inspection
4.15 Noncompliance
4.16 Premature Termination or Suspension of a Trial
4.17 Clinical Trial/Study Report
4.18 Multicentre Trial
5: Monitor’s Responsibilities
5.1 About this Chapter
5.2 Introduction
5.3 Monitoring
6: Safety & Adverse Event Reporting
6.1 Adverse Drug Reaction Reporting
7: Clinical Trial Protocol and Amendment
7.1 Trial Objectives and Purpose
7.2 Trial Design
7.3 Selection and Withdrawal of Subject
7.4 Treatment of Subject
7.5 Assessment of Efficacy
7.6 Assessment of Safety
7.7 Statistics
7.8 Direct Access to Source Data/Documents
7.9 Ethics
7.10 Financing and Insurance
7.11 Publication Policy
8: Investigator Brochure
9: Essential Documents
9.1 Archiving
9.2 Documents to be Present Pre-Study
9.3 Documents to be Added During the Study
9.4 Documents to be Added Post-Study
10 Example
10.1 Practical examples of good (and poor!) practice in relation to conducting clinical trial
ICH-GCP (E6-R2) international guidelines
(2) Advanced GCP training
1: Introduction to GCP
1.1 Background
1.2 What is GCP
1.3 New GCP Guideline
1.4 The Principles of ICH GCP
1.5 Some General Point
1.6 Documentation and Version Control
1.7 Quality Assurance
2: Competent Authorities (CA) and Independent Ethics Committee
2.1 Responsibilities of the CRA
2.2 Responsibility of the IEC
2.3 Subject Informed Consent Forms
2.4 Composition, Functions, Operations, Procedures and Records
2.5 How to avoid Ethics Committee issues
2.6. How to minimize safety issues
2.7. Measures to protect confidentiality of clinical trial subjects
2.8 Revisions and updates to the section on HIPAA and privacy.
3: Investigators
3.1 Investigator Responsibilities
3.2 Investigator Qualifications and Agreements
3.3 Adequate Resources
3.4 Medical Care of Trial Subjects
3.5 Communication with IRB/IEC
3.6 Compliance with the Protocol
3.7 Investigational Medicinal Products
3.8 Randomization Procedures and Un-blinding
3.9 Informed Consent of Trial Subjects
3.10 The best practices in obtaining informed consent
3.11 How to assess good oversight by a Principal Investigator
3.12 Records and Reports
3.13 Premature Termination or Suspension of a Trial
3.14 Progress Reports and Final Report(s) by Investigators
3.15 Archiving
3.16 В Considerations for the use of electronic systems in clinical trial management
3.17 Updated information on electronic records and use of EMRs in clinical research.
4: Sponsor’s Responsibilities
4.1 Quality Assurance and Quality Control
4.2 Contract Research Organization
4.3 Trial Design
4.4 Trial Management, Data Handling and Record Keeping
4.5 Investigator Selection
4.6 Financing
4.7 Notification/ Submission to Regulatory Authorities
4.8 Gaining CA approval in the EU
4.9 Confirmation of Review by IRB/IEC
4.10 Information on IM
4.11 What clinical trial processes should be covered by SOPs
4.12 The impact and principles of good vendor oversigh
4.13 Optimal management of IM
4.14 How to avoid Ethics Committee issue
4.15 Ensuring data quality by enhancing data management system
4.16 Manufacturing, Packaging, Labelling and Coding Investigational Products
4.17 Supplying and Handling Investigational Products
4.18 Record Access
4.19 Audit and Inspection
4.20 Noncompliance
4.21 Premature Termination or Suspension of a Trial
4.22 Clinical Trial/Study Report
4.23 Multicentre Trials
5: Monitor’s Responsibilies
5.1 About this Chapter
5.2 Introduction
5.3 Monitoring
5.4 Understand current thinking on risk based monitoring approaches and develop appropriate monitoring strategies for your study
5.5. Develop superior strategies for selecting sites, recruiting patients and motivating investigational site
5.6. Significantly improve your performance as a monitor to an advanced levels
5.7. Use effective planning and tracking tools to maximize efficiency as a monitoring
5.8. Develop strategies for dealing with complex monitoring issues
5.9.Gain expertise in monitoring oversight activities
6: Safety & Adverse Event Report
6.1 Adverse Drug Reaction Report
7: Clinical Trial Protocol and Amendments
7.1 Trial Objectives
7.2 Trial Design
7.3 Selection and Withdrawal of Subjects
7.4 Treatment of Subjects
7.5 Assessment of Effical
7.6 Assessment of Safe
7.7 Statistics
7.8 Direct Access to Source Data/Documents
7.9 Ethics
7.10 Financing and Insurance
7.11 Publication Policy
8: Investigator Brochure
9: Essential Documents
9.1 Archive
9.2В В Documents to be Present Pre-Study
9.3 Documents to be Added During the Study
9.4 Documents to be Added Post-Study
10. GCP audits and inspection
10.1The difference between audits and inspection
10.2 The types of inspections at a sponsor or CRO or investigational site
10.3 How best to prepare for an inspection
10.4 Best practice for conduct during an inspection
10.5 Common inspection findings and how to prevent their occurrence
10.6 How to respond to inspection findings
10.7 Construction of a plan for corrective and preventative actions
10.8 The most common findings in Health Authority GCP inspections
10.9 Review the regulations and guidance that governs clinical research compliance
10.10 Discuss GCP Auditing as a profession and how it differs from monitoring
10.11 Determine who gets audited and key factors and metrics for assessing when or why to audit
10.12 Explore how the FDA,EMEA,MHRA and local RB trains its inspectors to audit Clinical Investigators (Sites), Sponsors, and В Institutional Review Boards (IRB
10.13 Apply a quality-systems framework for assessing data and system
10.14 Implement data trend analysis to identify regulatory risk
10.15 Develop practical auditing skills using real-life audit example
10.16 Participate in role-play to enhance communication proficiency (Intake and Output
10.17 Communicate comprehensive findings with writing exercises and group discussion
11 Exam
11.1 Practical examples of good (and poor!) practice in relation to conducting clinical trial
12. Pharmacovigilance for Clinical Trial
A training package has been developed on the basis of the documents developed by ICH Steering Committee Members.
1) GCP course for Investigators and CRA
Trainers for Eastern European countries
Dr. Werner Gielsdorf, HSC- Germany
General Manager of TACIS project of European Commission in CIS, Manager of UNCTAD, WTO, ITC
EU, World Bank, UNCTAD/WTO
trainer of GCP, GLP, GDP,GMP
Dr.Zadorin Eugene, PhD,
International BioPharmaceutical Association
, Gerson Lehrman healthcare Council, First Clinical Research LLC Speaker
Bureau,head of the Department of Clinical Research of NBScience, Zintro Inc
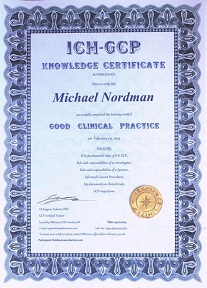
GCP certification
GCP certification is the formal recognition of clinical research professionals who have met professional eligibility requirements and demonstrated job-related knowledge and skills. The NBScience’s certification is granted in recognition of documented and verified work experience and successful performance on a multiple-choice exam
Program
Main principles of Good Clinical Practice
Regulatory acts of the European Union and International Conference of Harmonization
Responsibilities and the rights of the parties participating in clinical trial
Interaction of Sponsor and Investigator
Responsibilities of Investigator, Sponsor according to principles of Good Clinical Practice
Ethical aspects of clinical trials of medical products
Informed consent
File of Investigator; keeping of documentation
Legal and regulatory base of clinical trials of medical products in Europe and USA
FDA and EMEA
The basic requests to the documentation for clinical trials of medical product
Regulatory inspections of FDA
Types of inspection
Responsibilities of Sponsor, Investigator and Inspector at the time of audit
Specific clinical trials and GCP regulations in your country
Testing. GCP certification
Keywords: gcp training online,gcp test,gcp certification online,gcp online,gcp exam,online gcp,gcp certificate,ich gcp test,online gcp certificati
2) On-line training course on GCP audit and inspections
Overview
This GCP auditing course is designed to provide practical training resulting in a harmonised, common audit methodology in Europe and USA. The ICH GCP guideline implemented in the EU, Japan and the USA is being widely incorporated into guidelines worldwide. Systems audits, previously seen as advanced auditing, have become a basic task of many audit groups and are an essential element of inspections in Europe
The course material is regularly updated with the objective of experience sharing and a common professional approach in order to pave the way for mutual recognition and acceptance, reducing costs and stimulating efficiency, allowing faster medicinal product development to the benefit of the patients and health care