Stem Cell Therapy for Lyme Disease: A Promising Avenue for Treatment
1. Introduction: Lyme Disease and Its Challenges
Maladie de Lyme, caused by the bacterium Borrelia burgdorferi, is transmitted through the bite of infected black-legged ticks. It is one of the most common vector-borne diseases in North America and Europe. The condition can lead to a wide range of symptoms, including fever, fatigue, douleurs articulaires, neurological issues, et dans les cas graves, chronic debilitating symptoms that persist long after the infection has been treated.
Traditionnellement, Lyme disease is treated with antibiotics, and early-stage Lyme disease can often be effectively cured with a course of these medications. Cependant, dans certains cas, particularly when the disease is not diagnosed promptly or the infection becomes chronic, patients may develop Post-Treatment Lyme Disease Syndrome (PTLDS). This syndrome is characterized by persistent symptoms such as fatigue, musculoskeletal pain, and neurological impairments, despite having undergone antibiotic therapy.
The persistent and debilitating nature of PTLDS has led researchers to seek alternative and more effective treatments for Lyme disease. One promising avenue of research is thérapie par cellules souches, which offers the potential to repair the damage caused by the disease and alleviate ongoing symptoms. Dans cet article, we explore how thérapie par cellules souches could help in the treatment of Lyme disease, particularly in cases where chronic symptoms persist.
2. Lyme Disease and Its Impact on the Body
Before diving into thérapie par cellules souches pour la maladie de Lyme, il’s essential to understand how the disease affects the body and why it can lead to long-term symptoms.
The Stages of Lyme Disease
- Early Localized Stage: The initial stage of Lyme disease typically occurs within three to 30 days after a tick bite. Common symptoms include a bull’s-eye-shaped rash, fièvre, fatigue, and muscle aches. At this stage, Lyme disease is often treatable with antibiotics.
- Early Disseminated Stage: If left untreated or inadequately treated, the bacteria can spread through the bloodstream, affecting other parts of the body such as the heart, système nerveux, and joints. This stage can involve symptoms like irregular heart rhythms, facial palsy (Bell’s palsy), and severe joint pain.
- Late Stage / Chronic Lyme Disease: Dans certains cas, the infection becomes chronic, with symptoms that can last for months or even years. Chronic Lyme disease, or PTLDS, often involves persistent fatigue, cognitive dysfunction (often referred to as « brouillard cérébral »), pain in the joints and muscles, and neurological issues. These symptoms are difficult to treat with conventional methods, leading many patients to seek alternative treatments.
3. Stem Cells and Their Role in Healing Lyme Disease
Thérapie par cellules souches offers a regenerative approach to healing tissues and improving the overall health of individuals suffering from chronic conditions like Lyme disease. Les cellules souches ont la capacité unique de se différencier en différents types de cellules, y compris les neurones, cellules musculaires, and cartilage, depending on the need of the body. In Lyme disease, thérapie par cellules souches can potentially address several aspects of the disease’s impact on the body.
How Stem Cells Help in Lyme Disease Treatment
- Réparation et régénération des tissus: Lyme disease can cause damage to various tissues in the body, including the joints, muscles, and nerves. Stem cells can differentiate into the specialized cells needed to repair and regenerate these damaged tissues, potentially improving function and reducing pain.
- Réduction de l'inflammation: Chronic Lyme disease is often associated with persistent inflammation, especially in the joints and nervous system. Stem cells have powerful anti-inflammatory properties that can help reduce inflammation, which is key to alleviating the pain and discomfort associated with PTLDS.
- Neurological Repair: One of the more serious complications of Lyme disease is its effect on the nervous system, causing symptoms like facial paralysis, memory issues, et dysfonctionnement cognitif. Stem cells can be used to repair damaged nerve tissue, favoriser la neurogenèse (growth of new neurons), and restore nerve function, which can help reverse some of the neurological damage caused by Lyme disease.
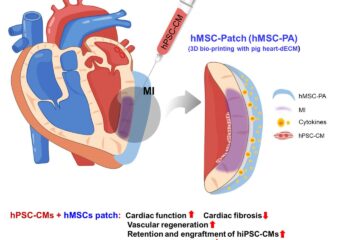
- Modulation du système immunitaire: Chronic Lyme disease can lead to an overactive or dysregulated immune response. Cellules souches, particularly mesenchymal stem cells (MSC), can help modulate the immune system, promoting a balanced immune response and reducing autoimmunity or inflammation.
4. Types of Stem Cells Used in Lyme Disease Treatment
There are several types of stem cells that can be used in the treatment of Lyme disease, each offering its own set of potential benefits:
Cellules souches mésenchymateuses (MSC)
Mesenchymal stem cells are one of the most commonly used stem cells for regenerative therapy, especially in the treatment of autoimmune and inflammatory conditions. These stem cells can be obtained from sources such as bone marrow, adipose (graisse) tissu, ou du sang de cordon ombilical.
MSCs have the ability to differentiate into multiple cell types, y compris les os, cartilage, and nerve cells. This makes them ideal for treating the musculoskeletal pain and neurological issues associated with Lyme disease. En plus, MSCs have anti-inflammatory properties and can help regulate immune system activity, which is essential for managing the chronic inflammation seen in Lyme disease.
Cellules souches pluripotentes induites (iPSC)
Induced pluripotent stem cells are a more advanced type of stem cell that can be generated by reprogramming adult cells (comme la peau ou les cellules sanguines) to an embryonic-like state. iPSCs are highly versatile, as they can develop into virtually any type of cell in the body. iPSCs are still being studied for their potential in various treatments, but they may eventually offer a way to generate tissues and cells that can repair damage caused by Lyme disease, especially in cases where nerve or organ tissue has been severely affected.
Cellules souches hématopoïétiques
Cellules souches hématopoïétiques, which are primarily found in bone marrow, are known for their ability to regenerate blood cells. While they are typically used in treatments for blood cancers and disorders, research is exploring their potential in Lyme disease therapy. They may play a role in improving immune function and tissue regeneration, especially in cases where Lyme disease has caused severe immune dysfunction.
5. Clinical Evidence and Research on Stem Cells for Lyme Disease
L'utilisation de thérapie par cellules souches for Lyme disease is still in its early stages, and much of the research is focused on animal models and small-scale human trials. Cependant, there are several studies that have shown promising results in using stem cells to treat Lyme disease, particularly in patients with chronic or neurological symptoms.
Études précliniques
Several animal studies have demonstrated the potential for stem cells to reduce inflammation, favoriser la réparation des tissus, and even reverse some of the neurological damage caused by Lyme disease. Par exemple, studies in mice have shown that mesenchymal stem cells can help repair damage to the nervous system and joints, leading to reduced pain and improved function.
Human Clinical Trials
Early-stage clinical trials have been conducted to assess the safety and efficacy of thérapie par cellules souches in patients with chronic Lyme disease and PTLDS. In these studies, patients have received stem cell injections or infusions, and many have reported improvements in pain levels, energy, et fonction cognitive. Cependant, more large-scale trials are needed to confirm these findings and develop standardized treatment protocols.
Thérapies combinées
Dans certains cas, thérapie par cellules souches is being combined with other treatments such as antibiotics or hyperbaric oxygen therapy (Hbot) to enhance the regenerative effects and support healing. This multi-modal approach may provide better outcomes for patients with complex, chronic Lyme disease.
6. The Future of Thérapie par cellules souches in Lyme Disease Treatment
Le potentiel de thérapie par cellules souches to treat Lyme disease, especially chronic Lyme and PTLDS, is vast. Alors que les recherches se poursuivent, we can expect more targeted and effective treatments that address the root causes of Lyme disease-related symptoms.
Thérapie par cellules souches may not only offer symptom relief but also play a role in regenerating damaged tissues, improving nerve function, and enhancing the body’s ability to fight off infection. À l'avenir, stem cell treatments may become a standard option for individuals suffering from the long-term effects of Lyme disease.
As with all emerging therapies, more research is required to fully understand the risks, avantages, and long-term effects of traitement des cellules souches pour la maladie de Lyme. Cependant, the initial evidence is promising, and many hope that stem cells could offer a new approach to treating one of the most challenging and complex diseases in modern medicine.
7. Conclusion: A Bright Future for Lyme Disease Treatment
Lyme disease is a complex illness that can lead to chronic symptoms that are difficult to treat with traditional methods. Thérapie par cellules souches represents a promising new frontier in the treatment of Lyme disease, offering the potential to repair damaged tissues, réduire l'inflammation, and improve neurological function.
Alors que la recherche en est encore à ses débuts, the results thus far suggest that stem cells could offer significant benefits to patients with chronic Lyme disease and PTLDS. As scientific understanding of thérapie par cellules souches advances, it could become a game-changer in the way we approach the treatment of Lyme disease and its long-term effects.
For patients who have not found relief through conventional therapies, thérapie par cellules souches offers hope for a future where Lyme disease can be effectively managed and even healed at its core.