Cellular Therapy: A Groundbreaking Approach for Autoimmune Remission
Cellular therapy has emerged as a revolutionary treatment strategy offering new hope for patients suffering from autoimmune diseases. These conditions, where the body’s immune system mistakenly attacks its own tissues, have long posed significant challenges to effective and lasting treatment. Traditional therapies often focus on managing symptoms or broadly suppressing immune activity, which can lead to unwanted side effects and limited remission periods. Cellular therapy, cependant, stands out by fundamentally transforming the immune system’s behavior, aiming for long-term remission and improved quality of life.
Understanding Autoimmune Diseases and the Need for Innovative Treatments
Autoimmune diseases encompass a wide range of disorders such as multiple sclerosis, polyarthrite rhumatoïde, lupus, et tapez 1 diabète. Despite their differences, they share the underlying problem of immune dysregulation. When the immune system becomes overactive or misdirected, it attacks healthy organs and tissues, causing inflammation, damage, and chronic symptoms.
Current standard treatments typically involve immunosuppressive drugs, steroids, or biologic agents that inhibit specific immune pathways. While these treatments can reduce disease activity, they rarely induce lasting remission and may compromise immune defenses against infections. Donc, the medical community has been in continuous search of more targeted and sustainable alternatives that can reset or recalibrate the immune system without broadly impairing its protective functions.
What Is Cellular Therapy and How Does It Work?
Cellular therapy refers to the use of living cells introduced into the patient to achieve a therapeutic effect. In the context of autoimmune diseases, one of the most promising forms of cellular therapy involves hematopoietic stem cell transplantation (GCSH). This approach essentially « resets » the immune system by first wiping out the dysfunctional immune cells through chemotherapy or radiation, and then infusing healthy stem cells that regenerate a new, ideally self-tolerant immune system.
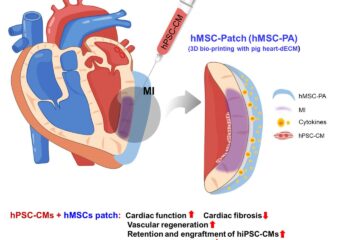
More recently, advanced techniques using regulatory T cells (Tregs) or mesenchymal stem cells (MSC) have been explored. These cells have natural immune-modulating properties and can help suppress autoimmune responses without compromising overall immune competence. Unlike broad immunosuppression, these therapies seek to restore immune balance and encourage remission by selectively targeting the root cause of autoimmune aggression.
Cellular Therapy: Exclusive Breakthrough for Autoimmune Remission
The real breakthrough of cellular therapy in autoimmune treatment is its potential to achieve long-lasting remission, a goal rarely realized with conventional treatments. Several clinical trials have reported encouraging results, particularly in diseases like multiple sclerosis and systemic sclerosis, where stem cell transplantation has induced extended periods of remission and even halted disease progression.
This exclusive breakthrough hinges on the ability of cellular therapy to reprogram the patient’s immune system. By regenerating a more tolerant immune profile, patients have experienced reduced flare-ups, lower medication dependence, and improved functional outcomes. For many, cellular therapy represents a paradigm shift from lifelong symptom management to possible disease modification and remission.
Advantages Over Traditional Autoimmune Treatments
1. Targeted Immune Resetting: Unlike immunosuppressive drugs that dampen the immune system broadly, cellular therapy selectively targets immune cells causing the disease without impairing overall immunity.
2. Potentiel de rémission à long terme: Clinical studies reveal that some patients achieve durable remission for years following treatment, reducing the need for continuous medication.
3. Reduced Side Effects: With advances in transplantation protocols and cell engineering, the risks of complications associated with cellular therapy are becoming more manageable.
4. Personalized Approach: Cellular therapies can be tailored to individual patient profiles, offering a more customized treatment pathway based on the type and severity of autoimmune disease.
Défis et orientations futures
Malgré sa promesse, cellular therapy for autoimmune diseases is still in a relatively early stage and not universally available. High costs, complex procedures, and the need for specialized medical centers limit widespread access. De plus, more extensive clinical trials are required to establish standardized protocols and long-term safety profiles.
Researchers are also investigating next-generation cellular therapies that use gene editing and synthetic biology to enhance therapeutic outcomes. Innovations such as CAR-T cells engineered to target autoimmune responses or off-the-shelf stem cell products could make these treatments more accessible and effective in the near future.
Conclusion
Cellular therapy signifies a transformative advancement in the treatment landscape for autoimmune diseases. By moving beyond symptom control to tackle the underlying immune dysfunction, it brings the promise of exclusive breakthroughs in achieving sustained autoimmune remission. As research progresses and technology evolves, cellular therapy has the potential to redefine hope and healing for millions affected by these chronic and often disabling conditions.