1) ARC, cCRA certification
2 Weeks
Maximum Allowed Duration: 3 Months
Expected Effort: 12 hours/week
Un associé de recherche clinique (ARC) is a professional who monitors clinical trials and research studies.
Benefits of Certified Clinical Research Associate Training & Attestation:
Commanditaires, CROs and other agencies involved in the implementation of clinical trials and other forms of medical research are increasingly looking for qualified individuals who have completed formal and approved training and certification in order to be able to rely on them to perform the tasks assigned to them.
CRA Training & Certification Program Structure:
Upon registering for the CRA Training and Certification program, members are granted access to the NBScience learning and certification platform. The online CRA Training & Qualification Program is a 24-hour standardized program that provides core clinical study learning. These are some of the important areas in which training is received after the qualification curriculum has been signed.
Introduction:
This study module, which consists of several lectures and presentations, introduces the participant to the pharmaceutical and clinical research industry.
It also allows for a thorough overview of the clinical research field and the development and developments that have led to the current clinical research environment. The Introductory Module also teaches individuals about clinical research stakeholders and the Principles of Good Clinical Practice (GCP). Technologies in the management of clinical trials are discussed in detail, and comprehensive knowledge of the major clinical research regulatory bodies that exist globally is also provided to individuals.
Drug Development:
This program consists of multiple lectures and includes instruction on the pre-clinical development of drugs and biologics, different stages of clinical drug development, design of clinical trials and endpoints in clinical trials.
Ethics in Drug Development:
Each series, consisting of multiple lectures, discusses the concept of ethics in clinical research, the Informed Consent Process, Evidence and HIPAA, and also offers instruction at the International Conference on Harmonization (je).
Regulations in Clinical Research:
This module provides training in FDA regulations such as 21 CFR Parts 11, 50, 54, 56, 312,812, et 814.
Roles & Responsabilités:
It is important to identify the roles of all stakeholders in the management of clinical trials so that standards that are realistic can be established. Each section provides a comprehensive overview of the roles of clinical practitioners, sponsors, suppliers and the Institutional Review Boards (CISR).
Documents essentiels:
Essential records are documents which, individually and collectively, make it possible to assess the conduct of the trial and the quality of the data generated. These records provide proof of the investigator’s compliance, support and evaluation with the Good Clinical Practice guidelines and all relevant regulatory requirements.
One of the most important and frequent inspection findings during investigator site inspections is the inadequacy of reliable and accurate source reporting. This is also the most common pitfall found during sponsor audits. To order to ensure that the results of the study are focused on reliable and relevant data, the value of good documentation practice needs to be stressed for the investigator sites. This curriculum focuses on the core principles of good data practice, offers intensive training to key areas such as source documentation, main documents, IND & NDA Requirements and the Clinical Study Report (CSR).
Study Start-Up:
Each section provides an overview of clinical procedures in the start-up phase of a clinical trial. A Study Start-Up Group, vendors and sites identified and activated, procedures established for data collection and reporting, and regulatory approvals obtained shall be established from the final procedure to the first patient visit. The program offers focused instruction in areas such as feasibility evaluation, site selection, pre-study visit, site initiation, recruitment and retention of participants, the TMF (Test Master File) and budgeting of clinical trials.
Study Monitoring & Close Out:
The monitor is responsible for “surveillance the conduct of a research project.” Research monitors must have a thorough understanding of the Code of Federal Regulations, local laws, guidelines and their assigned research protocols. A major part of the reporting duties is to inform and assist sites in compliance with FDA and other local and international regulations and/or recommendations, while also helping them meet the requirements of specific research studies. Monitors act both as communication channels between sites and sponsors and as supervisors for individual research projects. This program offers extensive training in areas such as regular site monitoring, CRF analysis and source data verification, product transparency and compliance, site closure, writing accurate monitoring reports and follow-up visit letters, and record archiving and maintenance.
Safety Reporting:
One of the CRA’s most important priorities is to ensure that clinical inspectors are fully aware of and comply with their responsibility for reporting adverse events. To do it, the CRA must often notify investigators of the criteria for adverse event reporting. Par conséquent, the CRA must be aware of both the regulatory and sponsor-specific criteria for reporting significant and non-serious adverse events in clinical trials. It requires the proper use and completion of adverse event forms and criteria and conditions for reporting adverse events that may go further than the regulatory requirements. Each program offers instruction in the identification and monitoring of adverse and serious adverse events in clinical trials.
Role of Quality Assurance & Data Management:
Each program offers relevant training in quality assurance (Assurance qualité) audits and testing, electronic data and signatures, information management and biostatistics..
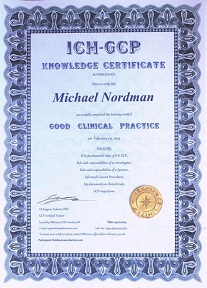
2) Cours GCP pour les enquêteurs et les ARC
3) Cours GCP pour les auditeurs
(voir ci-dessous ou pour des informations détaillées, cliquez ici)
Programme de formation GCP
(1) Formation GCP
ICH-GCP international guidelines
1: Introduction
1.1 Arrière-plan
1.2 Qu'est-ce que GCP ?
1.3 Nouveau guide GCP
1.4 Les principes de l’ICH GCP
1.5 Quelques points généraux
1.6 Documentation et contrôle de version
1.7 Assurance qualité
2: Autorités compétentes (Californie) et comité d’éthique indépendant (IE)
2.1 Responsibilities of the CUN
2.2 Responsibility of the IE
2.3 Formulaires de consentement éclairé du sujet (ICF)
2.4 Composition, Les fonctions, Opérations, Procedures and Record
3: Investigat
3.1 Responsabilités de l'enquêteur
3.2 Qualifications et accords des enquêteurs
3.3 Ressource adéquate
3.4 Soins médicaux des sujets d'essai
3.5 Communication with IRB/IE
3.6 Respect du protocole
3.7 Investigational Medicinal Produc
3.8 Procédures de randomisation et levée de l'aveugle
3.9 Consentement éclairé du sujet de l'essai
3.10 Dossiers et rapports
3.11 Résiliation ou suspension prématurée d'un procès
3.12 Rapports d'étape et rapport final(s) par les enquêteurs
3.13 Archivage
3.14 Considérations relatives à l'utilisation de systèmes électroniques dans la gestion des essais cliniques
3.15 Informations mises à jour sur les dossiers électroniques et l'utilisation des DME dans la recherche clinique.
4: Responsabilités du sponsor
4.1 Assurance qualité et contrôle qualité
4.2 Organisme de recherche sous contrat
4.3 Conception d'essai
4.4 Gestion des essais, Traitement des données et tenue de registres
4.5 Sélection des enquêteurs
4.6 Financement
4.7 Notification/ Submission to Regulatory Authoritie
4.8 Gaining CA approval in the
4.9 Confirmation of Review by IRB
4.10 Informations sur la messagerie instantanée
4.11 Fabrication, Emballage, Labelling and Coding Investigational Product
4.12 Supplying and Handling Investigational Product
4.13 Accès aux enregistrements
4.14 Vérification et inspection
4.15 Non-conformité
4.16 Résiliation ou suspension prématurée d'un procès
4.17 Rapport d'essai/d'étude clinique
4.18 Essai multicentrique
5: Responsabilités du moniteur
5.1 À propos de ce chapitre
5.2 Introduction
5.3 Surveillance
6: Sécurité & Déclaration des événements indésirables
6.1 Déclaration des effets indésirables des médicaments
7: Protocole d'essai clinique et amendement
7.1 Objectifs et but de l'essai
7.2 Conception d'essai
7.3 Sélection et retrait du sujet
7.4 Traitement du sujet
7.5 Évaluation de l'efficacité
7.6 Évaluation de la sécurité
7.7 Statistiques
7.8 Accès direct aux données/documents sources
7.9 Éthique
7.10 Financement et assurance
7.11 Politique de publication
8: Brochure de l'enquêteur
9: Documents essentiels
9.1 Archivage
9.2 Documents à présenter avant l'étude
9.3 Documents à ajouter pendant l'étude
9.4 Documents à ajouter après l'étude
10 Exemple
10.1 Des exemples pratiques de bonnes (et pauvre!) pratique relative à la conduite d'essais cliniques
I-GCP (E6-R2) directives internationales