الآليات الجزيئية والكيميائية الحيوية لتجديد القلب عبر الخلايا الجذعية: دور المواد الحيوية
مقدمة
أمراض القلب والأوعية الدموية (الأمراض القلبية الوعائية) تظل السبب الرئيسي للوفيات على مستوى العالم. رغم التقدم في العلاج الطبي, قدرة القلب على التجدد الجوهرية محدودة, خاصة بعد احتشاء عضلة القلب (مي). ظهرت العلاجات المعتمدة على الخلايا الجذعية كوسيلة واعدة لإصلاح وتجديد أنسجة القلب التالفة. لكن, تحديات مثل ضعف بقاء الخلية, نقش محدود, وعدم كفاية التكامل الوظيفي يعيق تطبيقها السريري. تم تحديد المواد الحيوية كمكونات حاسمة في تعزيز العلاج بالخلايا الجذعية من خلال توفير بيئة دقيقة داعمة تعزز بقاء الخلية., التمايز, وتكامل الأنسجة.
1. المواد الحيوية في إصلاح القلب القائم على الخلايا الجذعية
1.1 أهمية المواد الحيوية
تعمل المواد الحيوية كسقالات تدعم ارتباط الخلايا الجذعية, الانتشار, والتمايز. أنها تحاكي المصفوفة خارج الخلية (إدارة المحتوى في المؤسسة) من أنسجة القلب الأصلية, توفير الإشارات الهيكلية والكيميائية الحيوية الضرورية لتجديد الأنسجة. يجب أن تمتلك المواد الحيوية المثالية:
- التوافق الحيوي: غير سامة وغير مناعية.
- القابلية للتحلل البيولوجي: تتحلل بمعدل يتوافق مع تكوين الأنسجة.
- الخصائص الميكانيكية: تطابق صلابة عضلة القلب الأصلية لتسهيل الانكماش السليم.
- النشاط الحيوي: تعزيز التصاق الخلايا وتمايزها.
1.2 أنواع المواد الحيوية
- المواد الحيوية الطبيعية: الكولاجين, الليفين, حمض الهيالورونيك.
- المواد الحيوية الاصطناعية: بولي(حمض اللاكتيك المشارك الجليكوليك) (بلجا), بوليكابرولاكتون (PCL), البولي ايثيلين جلايكول (ربط).
- المواد الحيوية المركبة: مزيج من المواد الطبيعية والاصطناعية للاستفادة من مزايا كليهما.
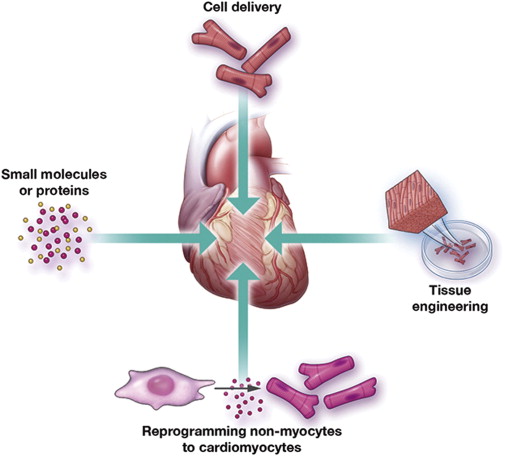
2. العلاج بالخلايا الجذعية في تجديد القلب
2.1 آليات العمل
تساهم الخلايا الجذعية في إصلاح القلب من خلال:
- التمايز المباشر: التحويل إلى خلايا عضلية القلب, الخلايا البطانية, أو خلايا العضلات الملساء.
- تأثيرات الباراكرين: إفراز العوامل النشطة بيولوجيا التي تعدل البيئة المحلية, تعزيز تكوين الأوعية الدموية, الحد من موت الخلايا المبرمج, وتعزيز إعادة تشكيل الأنسجة.
2.2 أنواع الخلايا الجذعية المستخدمة
- الخلايا الجذعية الجنينية (المجالس الاقتصادية والاجتماعية): خلايا متعددة القدرات قادرة على التمايز إلى جميع أنواع الخلايا.
- الخلايا الجذعية المحفزة (iPSCs): إعادة برمجة الخلايا الجسدية بقدرات متعددة القدرات.
- الخلايا الجذعية الوسيطة (اللجان الدائمة): خلايا متعددة القدرات ذات خصائص مناعية.
- الخلايا السلفية القلبية (تكلفة النقرة): الخلايا التي لديها القدرة على التمايز إلى أنواع خلايا القلب.
3. الآليات الجزيئية والكيميائية الحيوية
3.1 مسارات الإشارات
يتم تنظيم تمايز الخلايا الجذعية ووظيفتها من خلال العديد من مسارات الإشارات الرئيسية:
- مسار Wnt/β-catenin: تشارك في تمايز عضلة القلب.
- إشارة الشق: ينظم قرارات مصير الخلية أثناء نمو القلب.
- البروتينات المورفولوجية للعظام (مركبات قتال المشاة): تعزيز تمايز الخلايا السلف القلب.
- عوامل نمو الخلايا الليفية (صناديق الأجيال القادمة): تحفيز تكوين الأوعية الدموية وإصلاح الأنسجة.
3.2 إشارات باراكرين
تفرز الخلايا الجذعية عوامل مختلفة تؤثر على البيئة الدقيقة للقلب:
- عامل نمو بطانة الأوعية الدموية (VEGF): يعزز تكوين الأوعية الدموية.
- عامل نمو خلايا الكبد (HGF): يحفز تكاثر الخلايا وبقائها.
- عامل النمو الشبيه بالأنسولين (منتدى إدارة الإنترنت): يعزز نمو الخلايا وتمايزها.
4. سقالات المواد الحيوية الهندسية لتوصيل الخلايا الجذعية
4.1 اعتبارات تصميم السقالة
وينبغي السقالات الفعالة:
- تقليد ECM: توفير بنية ثلاثية الأبعاد تدعم نمو الخلايا.
- دمج الجزيئات النشطة بيولوجيا: إطلاق عوامل النمو لتعزيز وظيفة الخلايا الجذعية.
- تكون موصلة للكهرباء: تسهيل مزامنة خلايا عضلة القلب المشتقة من الخلايا الجذعية مع الأنسجة المضيفة.
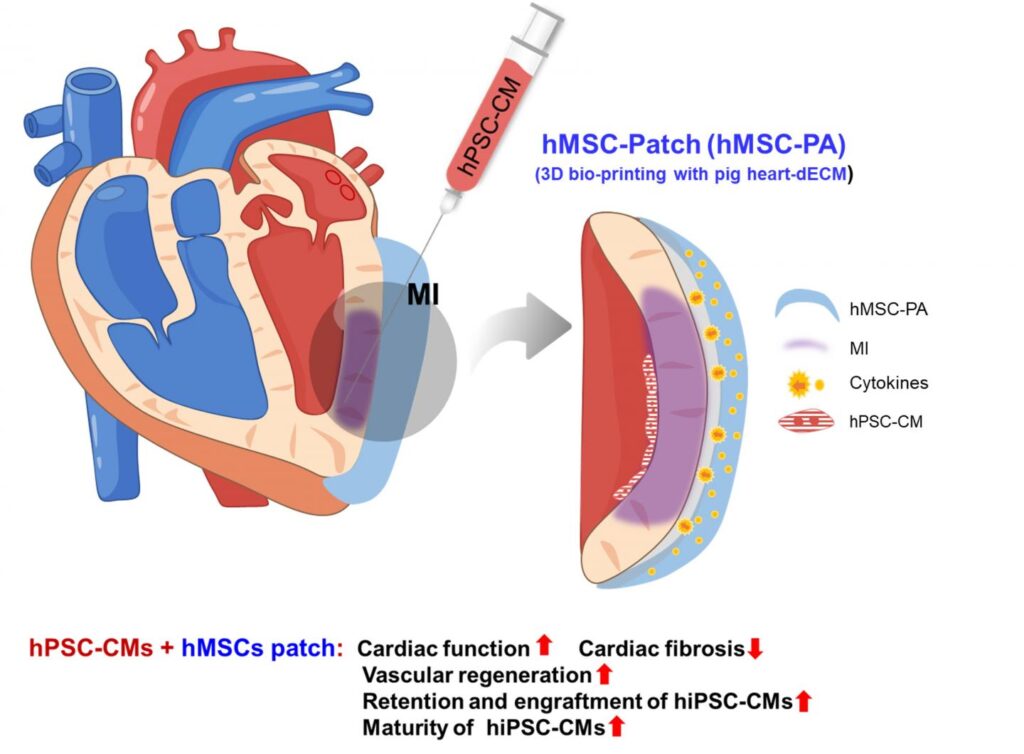
4.2 أنظمة التسليم
- الهلاميات المائية القابلة للحقن: السماح بالولادة بأقل تدخل جراحي والتوافق مع المنطقة المصابة بالاحتشاء.
- صفائف ميكرونيدل: توفير إطلاق خاضع للرقابة للخلايا والعوامل النشطة بيولوجيا.
- 3د السقالات المطبوعة: توفير تحكم دقيق في بنية السقالة وتكوينها.
5. التحديات في تصميم المواد الحيوية لتطبيقات القلب
على الرغم من التقدم, لا تزال هناك العديد من التحديات:
- محاكاة البيئة المكروية للقلب الأصلية: من الصعب تكرار بنية القلب ووظيفته المعقدة.
- ضمان استقرار السقالة على المدى الطويل: يجب أن تتحلل المواد بمعدل يتناسب مع تكوين الأنسجة.
- تحقيق التكامل الوظيفي: يجب أن تتكامل السقالات كهربائيًا وميكانيكيًا مع الأنسجة المضيفة.
6. الاتجاهات المستقبلية في تطوير المواد الحيوية
- المواد الحيوية الذكية: الاستجابة للمحفزات البيئية (على سبيل المثال., الرقم الهيدروجيني, درجة حرارة).
- الطباعة الحيوية: إنشاء هياكل الأنسجة المعقدة بدقة عالية.
- تحرير الجينات: تعزيز وظيفة الخلايا الجذعية من خلال تقنية كريسبر/كاس9.
7. خاتمة
تلعب المواد الحيوية دورًا محوريًا في تعزيز فعالية العلاجات القائمة على الخلايا الجذعية لتجديد القلب. من خلال توفير بيئة دقيقة داعمة, أنها تسهل بقاء الخلايا الجذعية, التمايز, والاندماج في الأنسجة المضيفة. يعد البحث والتطوير المستمر في علوم المواد الحيوية ضروريًا للتغلب على التحديات الحالية وترجمة هذه العلاجات إلى ممارسة سريرية.
مراجع
- كامبريا, ه., وآخرون. (2017). العلاج بالخلايا الجذعية القلبية الترجمية: التقدم من الجيل الأول إلى أنواع خلايا الجيل التالي. npj الطب التجديدي, 2, 17. https://www.nature.com/articles/s41536-017-0024-1
- فانغ, ج., وآخرون. (2022). هندسة علاجات الخلايا الجذعية لإصلاح القلب. مراجعات الطبيعة لأمراض القلب, 19(10), 613-630. https://pubmed.ncbi.nlm.nih.gov/35863282/
- فاسو, س., وآخرون. (2021). النهج القائم على المواد الحيوية لتجديد القلب. الحدود في الهندسة الحيوية والتكنولوجيا الحيوية, 9, 671. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8636758/
- ليو, م., وآخرون. (2025). تجديد وإصلاح القلب: الآليات الجزيئية. مراجعات الطبيعة لبيولوجيا الخلايا الجزيئية, 26(1), 1-15. https://www.nature.com/articles/s41580-024-00792-2
الصور


